Mobility Autonomy In CCRCs: From Private Cars, Community Transport Models, To Aging In Place
- Senior Living+Studio

- Sep 30, 2025
- 14 min read
Introduction – The Autonomy Crisis

Margaret had driven herself everywhere for 63 years. At 84, living independently in her CCRC's cottage-style residence, her car represented far more than transportation—it was spontaneity, identity, and proof that age hadn't diminished her capability. Then came the medication adjustment that affected her depth perception, the minor fender-bender in the parking lot, and the conversation with her daughter that ended with surrendered keys.
Within weeks, Margaret's world contracted. Medical appointments required advance coordination. Spontaneous coffee with friends downtown became complicated logistics. The Thursday evening book club she'd attended for five years—now a burden she eventually abandoned. Her daughter, juggling her own career and family, grew resentful of constant chauffeur duty. Margaret felt she'd lost more than driving privileges; she'd lost her place in the world.
This story repeats itself across continuing care retirement communities with heartbreaking regularity. CCRCs promise "aging in place"—the ability to remain in a community through changing care needs—yet most fail to anticipate or design for the mobility crisis that inevitably arrives. We build parking lots assuming residents will drive indefinitely, then scramble to retrofit transportation solutions when the car keys disappear. Mobility isn't just logistics; it's the psychological infrastructure of independence.[^1]

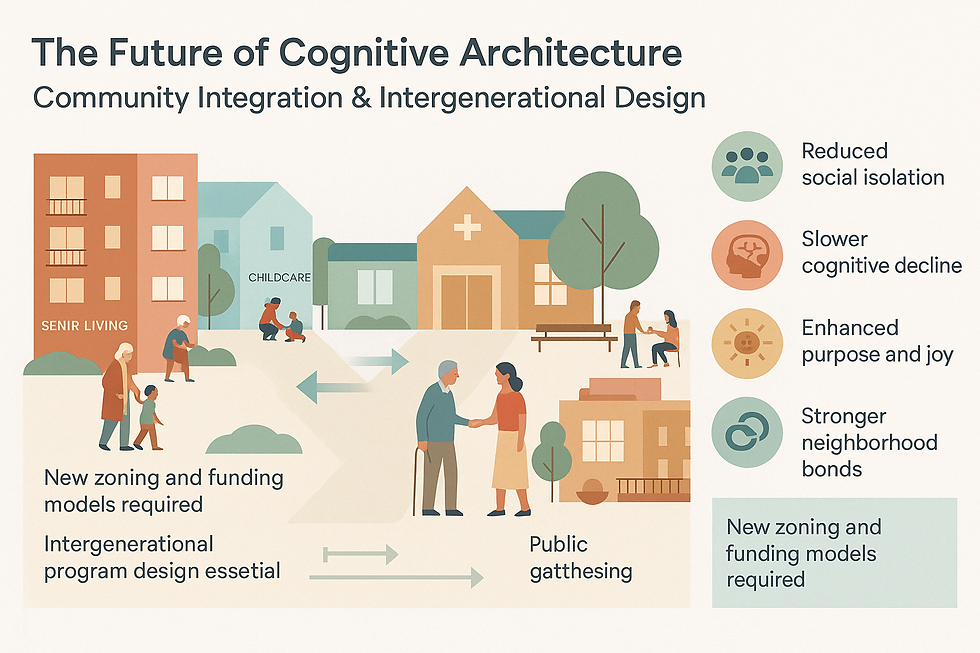
The thesis is straightforward: Communities that proactively build multi-modal mobility ecosystems—integrating walkability, shared transport, technology, and cultural transformation—can sustain resident autonomy throughout the aging continuum. The question isn't whether residents will stop driving, but whether we've designed communities that allow them to thrive when they do.
Understanding the Mobility Continuum
Resident transportation needs evolve through three distinct phases, each requiring different infrastructure and support:
Phase 1: Independent Driving. New residents arrive with personal vehicles, often trading larger family homes for CCRC living while maintaining complete mobility independence. Driving represents normalcy, continuity with their pre-retirement identity. Communities accommodate this phase well—visitor parking, resident garages, adequate roadways. The assumption that this phase lasts indefinitely becomes our first planning failure.
Phase 2: Transition. This is the most emotionally fraught stage. Cognitive changes, medication side effects, vision or hearing decline, and physical frailty make driving progressively riskier. According to the National Highway Traffic Safety Administration, drivers aged 70 and older have higher crash death rates per mile traveled than middle-aged drivers, with rates increasing notably after age 80.[^2] The Centers for Disease Control and Prevention reports that older adults are more likely to be killed or hospitalized following motor vehicle crashes compared to younger drivers, partly due to age-related fragility and medical complications.[^3]
Yet the transition isn't binary. Many residents drive selectively—daytime only, familiar routes, avoiding highways or bad weather—before stopping entirely. This partial autonomy phase demands flexible policies and infrastructure that few communities provide. Instead, we often force all-or-nothing decisions: full driving privileges or complete dependence on alternatives.

Phase 3: Post-Driving. Residents rely entirely on community shuttles, family members, rideshare services, or walkable amenities. Success in this phase determines whether aging in place means thriving or merely surviving. The gap between Phase 1 infrastructure investment (parking, roads) and Phase 3 infrastructure investment (transit systems, walkability, connectivity) represents the autonomy deficit plaguing most CCRCs.
The Safety Imperative – Supporting Informed Decision-Making
Communities have a responsibility to help residents navigate mobility transitions safely, and this requires more than passive observation. Driving cessation isn't simply about reducing liability; it's about protecting residents' wellbeing while preserving dignity.
Feller & Wendt, a reputable and established personal senior advocate law firm serving Utah, Idaho, and Arizona that works extensively in the senior living industry providing teaching, seminars, community outreach, protecting seniors' rights, published comprehensive guidance on aging and driving safety—not from a litigation perspective, but from a prevention and protection standpoint. Their investment in education demonstrates how seriously the sector must take age-related driving risks.
Their guide addresses critical factors that CCRCs should integrate into resident wellness programming: medication interactions that impair reaction time and judgment; vision and hearing changes that affect hazard perception; cognitive decline that impacts decision-making; self-assessment tools for residents and families; adaptive technologies that can extend safe driving; and conversation frameworks for families navigating this sensitive transition.

When legal advocates who typically represent injured parties invest resources in preventing harm to older drivers, it underscores both the seriousness of age-related driving risks and the importance of proactive planning. Research from the National Institute on Aging confirms that multiple medications, particularly those affecting the central nervous system, significantly increase crash risk among older adults.[^4] This isn't about restricting independence—it's about equipping residents and families with information before a crisis forces hasty decisions.
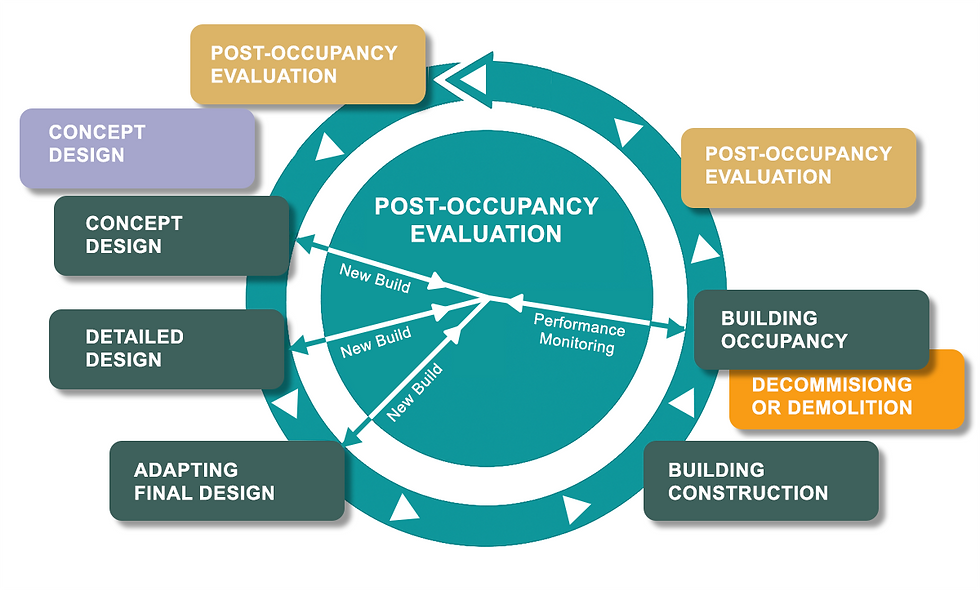
This educational approach should be standard in CCRCs. Communities must shift from reactive crisis management (removing driving privileges after incidents) to proactive support (providing assessment resources, facilitating family conversations, building robust alternatives). The question becomes: if we know the transition is inevitable, why do we wait for accidents to address it?
The Cost of Inadequate Mobility Design
When communities fail to design for the post-driving phase, the consequences cascade through every dimension of resident life and community operations.
Social isolation intensifies. Residents who can't drive and lack convenient alternatives progressively withdraw. The off-campus restaurant they loved, the downtown theater, the specialist physician across town—all become inaccessible. Studies show that transportation barriers are among the strongest predictors of social isolation among older adults, which correlates with increased mortality, depression, and cognitive decline.[^5] We've inadvertently designed loneliness into our communities by assuming permanent automobile access.

Family relationships strain. Adult children become default chauffeurs, coordinating schedules around parents' medical appointments, grocery runs, and social activities. What begins as loving support often evolves into resentment and exhaustion. The AARP reports that family caregivers spend an average of 24 hours per month providing transportation assistance, time that conflicts with their own employment and family obligations.[^6] This burden contributes to premature decisions to relocate parents to higher-acuity settings.
Premature moves accelerate. Residents who can't navigate community life without personal vehicles sometimes choose to leave for facilities offering more comprehensive services—even when their medical needs don't justify the transition. We lose residents not because they require skilled nursing, but because we failed to design mobility alternatives that preserve independence. This represents both a quality-of-life failure and a business sustainability issue.
Reputational consequences accumulate. Word spreads among prospective residents: "It's fine if you can drive, but don't plan on staying once you can't." Communities gain reputations as car-dependent, deterring forward-thinking prospects who understand their own aging trajectory. In an increasingly competitive senior living market, mobility infrastructure becomes a differentiator.
Consider a composite example drawn from industry experience: A well-appointed CCRC in the Southwest offered exceptional amenities—fitness center, fine dining, healthcare clinic—but located them across a sprawling 40-acre campus connected by winding roads with minimal sidewalks. When residents could no longer drive the quarter-mile from cottages to the main building, satisfaction scores plummeted. The twice-daily shuttle proved inadequate for spontaneous socialization. Within three years, the community faced declining occupancy as residents left for more compact, walkable competitors.
Designing the Mobility Ecosystem – Four Pillars
Solving the mobility crisis requires integrated strategies across site planning, transportation systems, technology, and culture. These four pillars work synergistically; implementing only one or two produces marginal improvements.
Pillar 1: Site Planning for Walkability
The foundation of mobility autonomy is compact, mixed-use site design. When independent living, assisted living, dining venues, wellness facilities, healthcare services, and retail are within comfortable walking distance, residents maintain autonomy throughout the aging continuum.
Universal design principles must guide pedestrian infrastructure: sidewalks wide enough for walkers and wheelchairs to pass comfortably (minimum 5 feet, ideally 6-8 feet); frequent benches at 200-300 foot intervals for rest stops; shade structures or tree canopies protecting from sun exposure; clearly marked, level crossings that don't require navigating curbs; minimal grade changes, with ramps meeting ADA standards where elevation changes are necessary.[^7]
Cognitive wayfinding deserves special attention. As residents experience early memory changes, environmental cues become critical navigation tools. Design should incorporate clear sightlines between destinations, intuitive paths that minimize decision points, landmark-based navigation using distinctive architectural features or landscaping, consistent directional signage with large, high-contrast text, and lighting that provides security without glare or disorientation.

The parking-versus-pedestrian balance requires reconsideration. Traditional CCRC master planning prioritizes automobile circulation and parking, often pushing buildings apart to accommodate surface lots. Forward-thinking communities flip this hierarchy: structured or peripheral parking liberates the community core for pedestrian-oriented development. Residents may walk past parked cars, but they walk through activated, pleasant environments to reach destinations.
One successful example: A Colorado CCRC clustered all residential buildings, dining, wellness, and services within a landscaped, traffic-free quarter-mile loop. Residents could walk safely to every amenity, with golf carts available for those with mobility limitations. When driving became impractical, residents' daily routines continued uninterrupted. The design decision made during master planning prevented the isolation crisis that other communities address through expensive, partial retrofits.
Pillar 2: Community Transport Systems
Even optimally walkable communities require transportation for off-campus destinations: medical appointments, shopping, cultural events, places of worship, family visits. Robust transport systems preserve the spontaneity and reach that personal vehicles provided.

Scheduled shuttle services form the baseline. Routes should connect to essential destinations: grocery stores, medical centers, downtown districts, shopping areas, cultural venues, religious institutions. Frequency matters enormously—hourly service provides utility; twice-daily service provides frustration. Vehicles must be accessible (low-floor or lift-equipped) with comfortable seating and climate control. Drivers require training not just in safe operation but in assisting passengers with mobility aids and cognitive support needs.
On-demand rideshare partnerships complement scheduled routes by enabling spontaneous trips. Integration with Uber, Lyft, or specialized senior transportation services (with community-negotiated rates or subsidies) provides flexibility. However, implementation requires attention to the digital divide; not all residents use smartphones comfortably. Concierge services that book rides by phone or in-person request become essential accessibility accommodations.
Community vehicle pools serve residents in the transition phase who drive occasionally but no longer need personal cars. A fleet of three to five vehicles reserved through the front desk or app enables grocery runs, brief errands, or visits when shuttle schedules don't align. This option preserves driving capability while reducing the financial and maintenance burden of ownership. Appropriate screening (valid license, recent assessment) manages risk while supporting partial autonomy.
Volunteer driver programs leverage the resident community itself. Residents who remain comfortable driving assist neighbors with transportation needs, fostering social bonds while providing service. Programs require careful structure: background checks, insurance verification, mileage reimbursement, training on passenger assistance, and clear policies about limitations (no medical transport requiring lifting, for example). When implemented well, these programs strengthen community cohesion while expanding mobility options.
The key insight across all transport options: we're not just moving people from Point A to Point B. We're attempting to preserve the spontaneity that driving provided—the ability to decide "I'll go to the bookstore this afternoon" without days of advance planning. Systems must be flexible and responsive, not just functional. Research consistently demonstrates that transportation availability directly correlates with life satisfaction and social engagement among older adults who no longer drive.[^8]
Pillar 3: Technology & Communication Tools
Technology enables mobility ecosystems to function efficiently, but implementation must account for varying comfort levels and universal design principles.

User-friendly scheduling platforms should offer multiple access points: smartphone apps for tech-comfortable residents; computer-based booking systems in common areas with large monitors and simplified interfaces; tablet stations in residential buildings; phone-based concierge service for those uncomfortable with digital tools; and even paper reservation forms for those who prefer analog processes. The principle: technology should expand access, never create barriers.
Real-time tracking capabilities reduce anxiety and wait times. When residents can see shuttle locations and estimated arrival times (similar to public transit apps), they plan more confidently and wait more comfortably. Digital displays in building lobbies supplement personal devices, serving residents who don't carry smartphones.
Wayfinding applications designed for older adults help residents navigate both on-campus and off-campus destinations. Features should include: extra-large text and buttons, voice guidance, simplified maps emphasizing landmarks over street grids, integration with health conditions (suggesting routes with frequent rest stops for residents with cardiac concerns, for example), and offline functionality for areas with poor cellular coverage.
Digital literacy support transforms technology from obstacle to enabler. Regular training sessions (small groups, patient instruction, hands-on practice), one-on-one technology coaching, peer mentorship programs (tech-comfortable residents teaching neighbors), and ongoing support (not just initial training) ensure that tools intended to help don't inadvertently exclude.
Critical caveat: Technology must augment, never replace, human-centered service. The 24-hour concierge desk that answers questions, makes exceptions, and provides reassurance remains essential. Automated systems should enhance options, not become the sole access point. We're designing for humans experiencing cognitive changes, sensory decline, and learned technological patterns from different eras. Flexibility and redundancy aren't inefficiencies—they're accessibility imperatives.
Pillar 4: Cultural Shift & Transition Support
Infrastructure alone cannot solve the mobility crisis; community culture must normalize driving cessation as a natural aging transition rather than a shameful failure.
Proactive assessment programs reframe the conversation. Occupational therapy-led driving evaluations—voluntary, non-punitive, focused on safety rather than judgment—provide objective information that depersonalizes difficult decisions. When offered as wellness programming ("Let's assess your driving safety, just like we assess your balance and strength"), resistance decreases. These assessments identify specific limitations (night driving, highway merging) that might allow continued selective driving rather than forcing complete cessation.
"Driving retirement" recognition programs honor the decision as responsible and praiseworthy. Small ceremonies, newsletter recognition, or private acknowledgments from leadership validate the courage required. Some communities create "Emeritus Driver" designations with special parking for when family members drive residents' cars. These symbolic gestures counter the shame and loss many residents feel.
Peer mentorship initiatives connect residents who've successfully transitioned with those currently facing the decision. Hearing a neighbor explain "I was terrified to give up my keys, but here's how I've stayed connected" normalizes the experience and provides practical strategies. These conversations carry weight that staff guidance cannot match.
Family education brings adult children into the planning process early. Workshops on having difficult conversations, understanding age-related driving risks, and exploring alternatives reduce the crisis-driven arguments that fracture relationships. Communities can share educational resources—such as the Feller & Wendt driving safety guide or materials from professional associations—as part of wellness programming, framing the transition as safety and self-care rather than loss of independence.

The American Geriatrics Society provides evidence-based guidelines for assessing older drivers that balance safety with autonomy, emphasizing individualized evaluation rather than age-based restrictions.[^9] Incorporating these professional standards into community policies demonstrates commitment to informed, compassionate decision-making.
Leadership modeling powerfully shapes community norms. When the executive director takes the shuttle to lunch, administrators walk to meetings, and department heads discuss their own families' driving transitions openly, non-driving becomes normalized rather than stigmatized. Residents observe these behaviors and internalize: "Successful, capable people don't always drive themselves—maybe I don't need to either."
Culture change requires time, consistency, and authentic commitment. It cannot be manufactured through marketing language while operational reality communicates different values. If communities praise driving cessation publicly but provide inadequate alternatives, residents recognize the hypocrisy. Cultural transformation demands alignment between stated values and lived experience.
The Case for ROI – Why This Matters to Operators
Investing in comprehensive mobility ecosystems delivers measurable returns across resident satisfaction, operational efficiency, and market positioning.
Resident retention extends. When residents can maintain independent, engaged lives without personal vehicles, they remain in independent or assisted living longer rather than transitioning prematurely to higher-acuity (and often off-campus) settings. Extended residency duration stabilizes revenue, reduces turnover costs, and improves community cohesion. Industry data suggests that transportation satisfaction ranks among the top five factors influencing resident retention decisions.
Market differentiation strengthens. As baby boomers—who expect technological integration, environmental sustainability, and person-centered services—become the primary CCRC demographic, mobility infrastructure becomes a competitive advantage. Prospects increasingly ask sophisticated questions during tours: "What happens when I can't drive?" Communities with comprehensive answers win contracts; those offering vague reassurances lose to competitors.
Regulatory alignment improves. Proactive mobility planning may reduce liability exposure related to resident driving incidents on campus (though this should not be the primary motivation). More significantly, it demonstrates alignment with emerging person-centered care standards and quality metrics. Accreditation bodies increasingly evaluate transportation adequacy as a component of holistic wellbeing support.
Operational efficiency gains. Robust transportation systems reduce ad-hoc staff time spent arranging emergency rides, managing resident complaints about isolation, or coordinating with frustrated family members. Maintenance and security staff spend less time managing parking conflicts, vehicle incidents, or abandoned cars. These efficiency gains free staff to focus on value-added resident services.
Reputation and referral patterns improve. Families and residents notice whether the community feels vibrant and engaged or isolated and dormant. Mobility infrastructure directly influences this perception. Residents who can easily access off-campus activities, maintain medical appointments, and visit family remain more socially connected, physically active, and cognitively engaged—the visible indicators of quality that drive word-of-mouth referrals.
Financial modeling should calculate these returns holistically: decreased turnover costs (typically 3-6 months of revenue per unit), increased occupancy from market differentiation (1-2% occupancy improvement significantly impacts revenue), reduced family complaints and associated staff time (harder to quantify but operationally significant), and potential premium pricing for mobility-forward communities (prospects may pay 5-10% more for demonstrably superior transportation infrastructure).
The investment required—master planning for walkability, shuttle fleet and operations, technology platforms, cultural programming—pales compared to the costs of poor mobility infrastructure: empty units, dissatisfied residents, staff turnover from frustration, and reputational damage that affects years of future census.
Conclusion – Reframing Mobility as Care Infrastructure

Mobility isn't an amenity, like a second pool or upgraded finishes. It's foundational infrastructure for dignity, autonomy, and successful aging in place. Yet we continue designing CCRCs as if residents will drive indefinitely, then scrambling to retrofit partial solutions when reality intervenes.
The industry standard must shift: mobility ecosystems should be integral to master planning from the first schematic design, not afterthoughts addressed during operational problem-solving. This requires breaking the mental model that parking lots and roadways constitute "transportation infrastructure" while dismissing sidewalks, shuttles, and wayfinding as soft amenities. In communities designed for aging populations, the reverse is true—pedestrian and transit infrastructure is essential; parking is supplementary.
We challenge CCRC operators to audit current mobility offerings through the resident journey lens. Ask honestly: "If I couldn't drive tomorrow, could I maintain my independence, social connections, and spontaneity in this community?" If the answer produces hesitation, the infrastructure gap demands attention.
The residents entering CCRCs today will live there for 15-20 years on average, spending the majority of that time in the post-driving phase. Will we design communities that enable thriving throughout that continuum, or will we continue forcing residents to choose between premature dependence and unsafe driving? The question answers itself once we recognize that mobility autonomy isn't about transportation—it's about whether we truly understand what "aging in place" means.
Communities that build multi-modal mobility ecosystems don't just manage aging; they create environments where residents can continue growing, contributing, and living fully regardless of whether they hold car keys. That's the promise of continuing care we should deliver.
Key Takeaways
Mobility transitions are inevitable, not exceptional. Most CCRC residents will spend the majority of their residency in the post-driving phase. Design and operations must prioritize this reality rather than treating it as an edge case.
Infrastructure integration precedes cultural acceptance. Asking residents to surrender car keys without providing robust alternatives guarantees resistance and failure. Build the ecosystem first; the cultural shift follows when residents experience viable options.
Walkability is primary infrastructure, not landscaping. Compact, mixed-use site planning with universal design pedestrian networks should drive master planning decisions, not parking lot optimization.
Transportation must enable spontaneity, not just scheduled access. The difference between twice-daily shuttles and hourly service with on-demand options is the difference between managing decline and preserving independence.
Technology expands access only when universally designed. Digital platforms must complement, never replace, analog alternatives. The oldest, least tech-comfortable residents should find systems as accessible as the youngest, most digitally native staff.
Leverage community resources and mission-driven advocates. CCRCs should connect residents and families with local Departments of Motor Vehicles (for driver assessments and voluntary ID programs), state Long-Term Care Ombudsman offices (for rights advocacy and problem resolution), AARP chapters (for educational resources and community programs), and local senior living advocates such as Feller & Wendt where they are mission-driven to provide invaluable information to age in place—whether in communities or at home. These partnerships extend the support network beyond internal staff and demonstrate commitment to comprehensive resident wellbeing.
References
[^1]: National Highway Traffic Safety Administration. (2021). "Traffic Safety Facts: Older Population." U.S. Department of Transportation. DOT HS 813 196.
[^2]: National Highway Traffic Safety Administration. (2022). "Older Drivers: Motor Vehicle Crash Involvement and Fatality Risk." Traffic Safety Facts Research Note. DOT HS 813 228.
[^3]: Centers for Disease Control and Prevention. (2023). "Older Adult Drivers: Get the Facts." National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention.
[^4]: National Institute on Aging. (2020). "Medication Use and Older Drivers." NIH Publication No. 20-AG-7933. U.S. Department of Health and Human Services.
[^5]: National Academies of Sciences, Engineering, and Medicine. (2020). "Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System." Washington, DC: The National Academies Press.
[^6]: AARP Public Policy Institute. (2021). "Family Caregiving and Transportation: Challenges and Opportunities." Research Report. Washington, DC: AARP.
[^7]: U.S. Access Board. (2010). "ADA Accessibility Guidelines for Buildings and Facilities." U.S. Department of Justice, 36 CFR Part 1191.
[^8]: Journal of Aging and Social Policy. (2019). "Transportation and Quality of Life Among Older Adults: A Review of the Literature." Vol. 31, No. 4, pp. 287-310.
[^9]: American Geriatrics Society. (2019). "Clinician's Guide to Assessing and Counseling Older Drivers." 4th Edition. New York: American Geriatrics Society.
Feller & Wendt LLC, 1834 E 310 n, Layton, UT 80400, Utah/Arizona/Idaho https://www.fellerwendt.com/